Riding the Waves of ERP: When Therapy is the Storm
There’s a particular kind of quiet that settles over the room when a client understands ERP and agrees to an exposure for the first time. It’s not...
6 min read
KD HOLMES, LPC, EMDR CERTIFIED, BTTI TRAINED
:
Feb 21, 2023 8:51:52 AM

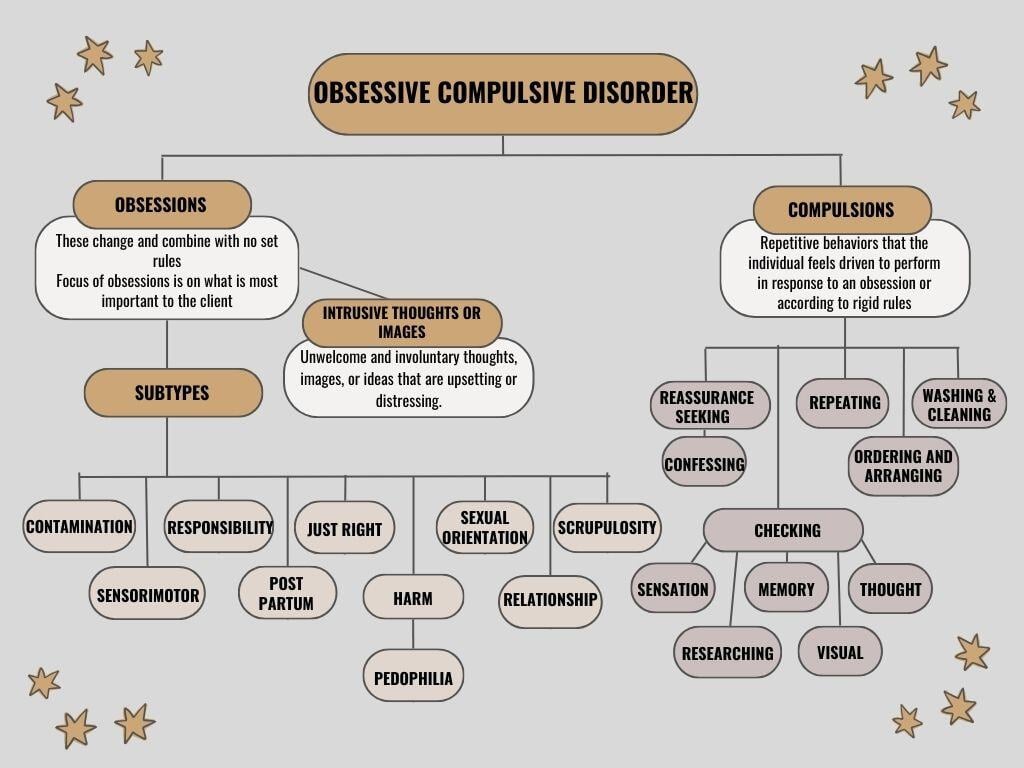
Obsessive-Compulsive Disorder (OCD) is characterized by persistent, unwanted obsessions and repetitive compulsions. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), obsessions refer to intrusive and distressing thoughts, images, or urges that cause significant anxiety. Compulsions are repetitive behaviors or mental acts that an individual feels driven to perform in response to these obsessions, often to reduce distress or prevent a feared event or situation. The cycle of obsessions and compulsions can be time-consuming and interfere with daily functioning, requiring professional treatment for effective management.
For sufferers it can feel like being trapped in a whirlwind of persistent, intrusive thoughts-obsessions-that generate intense unescapable fear and anxiety. To calm the storm, individuals often engage in repetitive behaviors-compulsions-to momentarily find relief. When one OCD loop ends, another often begins.
Despite being highly treatable, Obsessive-Compulsive Disorder (OCD) is frequently overlooked, misidentified, or misunderstood. This lack of awareness and understanding leaves many sufferers to carry their burden in solitude, feeling silenced by shame, fear of judgment, and overwhelming terror tied to their obsessions. These individuals often harbor intrusive and distressing thoughts that convince them they might be homicidal, pedophiles, or murderers. This isn't just a misinterpretation of their character; it's a debilitating mental health condition that distorts their perception of reality. The stigma surrounding these thoughts only adds to their isolation, making it crucial to foster greater awareness about OCD.
A study published in The Journal of Clinical Psychiatry revealed that primary care physicians misdiagnosed OCD in about 50.5% of cases. Misidentification was especially common in cases involving obsessions related to homosexuality (84.6%), aggression (80.0%), and fears of saying certain things (73.9%). Another systematic review emphasized that OCD is among the most disabling mental health disorders and is frequently misdiagnosed. This lack of recognition often leaves individuals with OCD undiagnosed for ten years or more.
Contrast this with Generalized Anxiety Disorder (GAD), which finds its roots in more grounded, everyday worries, though it may present with safety behaviors that superficially resemble OCD compulsions. The underlying experiences, however, diverge significantly. Similarly, Illness Anxiety Disorder is another distinct condition-marked by relentless fears of having a serious illness. Here, the individual’s worry manifests in compulsive behaviors, often without medical evidence to justify their concerns.
To untangle these nuances, I turn to tools such as Venn diagrams and, most importantly, draw from real-life experiences. These practices highlight differences not just as clinical distinctions, but as reflections of the human mind's differences.
OCD visited my professional life unexpectedly-due to my lack of proper training on the subject. Early in my career, I encountered a client with clear OCD symptoms. Yet, I missed the diagnosis. I simply didn’t have the training to recognize it or offer appropriate treatment. Even the psychiatrist involved failed to see it.
This was not an anomaly. My anxiety had an obsessive component, but no therapist I worked with for over a decade labeled it as such. I experienced OCD loops, obsessive thoughts, and intrusive images-but none met the criteria for an OCD diagnosis. I also had a personal encounter with Illness Anxiety Disorder, which heightened my insight into these conditions.
Each month now, clients with OCD arrive at my practice. Often, their stories are the same-they have been to other therapists, some for years, and yet their condition remained undiagnosed. This isn’t due to malice or neglect. Most therapists take their responsibilities seriously. We are rule followers who want to get it right. But the reality is clear-we have blind spots (or lack of training).
Whether you want to treat OCD being able to identify the disorder is crucial. Recognizing the symptoms allows you to understand when it's necessary to refer the individual to a specialist for ERP treatment. Early identification and referral can make a significant difference in the effectiveness of the treatment and the individual's overall well-being. OCD is treated with a specific protocol, much like other mental health issues. Research should guide treatment approaches to ensure effectiveness.
Therapists, we bear a profound responsibility to the individuals who entrust us with their mental health. For those with OCD, understanding the disorder and its treatment cannot be optional; it must stand as a professional imperative.
The gold standard for OCD treatment is ERP. ERP challenges both therapist and client to confront fear and anxiety head-on. This treatment requires exposing the client to their distressing triggers while simultaneously resisting the pull of compulsive behaviors used as temporary relief. We encourage our clients to confront their fears systematically. This process involves building a hierarchy of fears, starting with the least intense and gradually working up to the more significant ones. By facing these fears one step at a time, clients slowly build the confidence they need to manage anxiety and abstain from compulsive behaviors. This approach not only helps them address specific fears but also empowers them with the skills to handle obsessions more effectively. Through repeated exposure and practice, clients learn that they can navigate their fears and gain control over situations that once seemed overwhelming.
But herein lies the challenge. ERP stands in stark contrast to the reassurance-based practice that comes naturally to therapists-we are trained to comfort, to bring ease. Grasping the complexity of OCD and pushing ourselves (and our clients) down this counterintuitive path is critical to achieving real, lasting progress.
The International OCD Foundation (IOCDF) reports a 65-80% success rate for Exposure and Response Prevention (ERP) therapy in both children and adults. That statistic is truly remarkable.
At its core, ERP works because of the ILM, which has reframed our understanding of exposure therapies. These therapies were once thought to be effective because clients grew “desensitized” to their fears over time. However, recent insights reveal that the intensity and timing of exposures play a crucial role in the therapeutic process. The ILM teaches clients to reinterpret the relationship between fear and their responses, helping them guide their brains toward adopting a new narrative or a new learning.
Through this process, clients don't just “get used to” the presence of fear; instead, they begin to unlearn its overwhelming control. They replace that old pattern with a new learning experience that diminishes the power fear holds over them. This deeper understanding changes ERP from being simply a method of endurance into a tool of empowerment, offering clients the capacity to reshape their emotional responses and regain control over their lives. This model not only advances the effectiveness of therapy, making it more about growth and learning rather than mere survival and endurance.
Another foundational piece of ERP treatment is learning to live with uncertainty. For someone with OCD, this may not be the answer they want to hear, as it can be incredibly challenging to act opposite the need for certainty and ultimately control. However, embracing uncertainty is crucial for achieving the freedom they seek from obsessive thoughts and compulsive behaviors. By gradually exposing themselves to feared situations without resorting to compulsions, individuals can slowly build tolerance and acceptance of uncertainty. Over time, this process helps them realize that they can cope with anxiety and ambiguity, leading to a more fulfilling and less restricted life.
Exploring the intersection of Autism and OCD has been a bumpy road. Autistic individuals with OCD exhibit unique patterns that distinguish them from other OCD sufferers. Their repetitive behaviors, often referred to as "stimming," can sometimes be mistaken for compulsions, leading to misdiagnosis. Furthermore, the special interests that many autistic individuals possess can be misinterpreted as obsessive behaviors. Treating OCD in autistic individuals requires a nuanced approach, taking into account the sensory sensitivities that place an enormous strain on them. Traditional ERP methods can sometimes be overwhelming and counterproductive, potentially causing more harm than good. It's essential to adapt treatment strategies to the specific needs of autistic clients to ensure their well-being.
Continuous education on ERP is vital, yes, but improving as a profession also requires a shift in mindset. Recognizing OCD demands education and training to see obsessions and compulsions that meet the criteria for OCD. Beyond using our diagnostic eye and learning evidence-based approaches to treatment, we need to foster a culture of curiosity within ourselves-where every missed diagnosis becomes an opportunity to grow rather than a reason to retreat.
With ERP, we hold the key to a life-changing intervention-a way forward for those trapped in the relentless cycles of OCD. And with greater commitment, therapists can ensure that no one has to suffer through years of misdiagnosis when effective treatment is available.
To therapists witnessing clients struggling with intrusive thoughts, obsessions, and fears-I see you. Together, we can change the outcomes for these clients. The key is to begin by accurately identifying the symptoms of Obsessive-Compulsive Disorder (OCD) and then equipping clients with the right tools, Exposure and Response Prevention (ERP) therapy. This is just the beginning of the process for our clients, a journey that requires patience, understanding, and commitment. It's reminiscent of a concept often depicted in horror movies: you must name the fear or the monster for it to lose its power. Similarly, by naming OCD, we build insight for our clients and diminish the hold that these intrusive thoughts have on their lives. Through this method, we help them build confidence and relief.
Do not to become part of your client’s compulsions by reassuring them - this only reinforces their need for compulsions.
Do not under-treat your clients who do not want ERP by only engaging in talk therapy which does not have lasting effects on their symptoms.
Create an accepting environment where sufferers of OCD feel safe enough to share their experiences without fear of judgement, hospitalizations, or stigma attached.
Build your knowledge through education, and your consultation community. Check out our continuing Education live webinars Differentiating OCD and Anxiety Disorders (Part 1), The Art of Exposure and Response Prevention (Part 2), Understanding Neurodivergence and OCD, and Mastering Complex OCD Cases.

There’s a particular kind of quiet that settles over the room when a client understands ERP and agrees to an exposure for the first time. It’s not...

For therapists, grasping the nuanced distinctions between OCD and other anxiety disorders is vital for accurate diagnosis, leading to the most...
Obsessive-compulsive disorder (OCD) presents itself in nuanced, multifaceted ways. Subtypes of OCD can be conceptualized based on the nature of a...