Treating Developmental Trauma: Why Is It Important?
Trauma is a word that has been gaining more attention and importance in our society and in the therapy treatment world. We (therapists) all know what
5 min read
KD HOLMES, LPC, EMDR CERTIFIED, BTTI TRAINED
:
Jun 29, 2023 4:06:49 PM

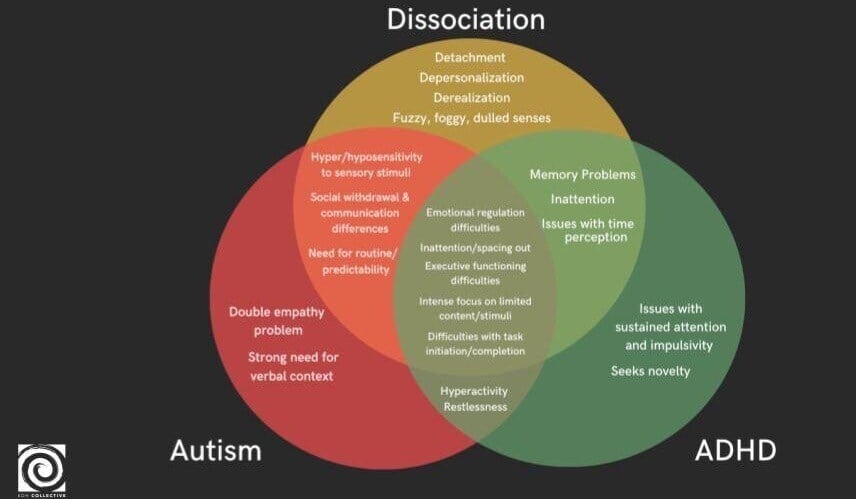
For therapists, trauma-informed care is of primary focus in our training and treatment. This approach, characterized by sensitivity to trauma and its effects, becomes especially critical when working with neurodivergent clients. Many individuals who are neurodivergent also grapple with the profound effects of trauma, creating a layered and complex intersection of challenges. The overlap between trauma symptoms and neurodivergent traits often makes therapeutic progress more nuanced, requiring us to become not only trauma-informed but also neurodivergent-informed.
While trauma-informed care is crucial, it can also lead to misdiagnosis when neurodivergent traits are mistakenly categorized as trauma-related symptoms. This misclassification can result in treatment approaches that aim to change these traits, further pathologizing our clients. For example, traits associated with Autism or ADHD might be seen as symptoms of trauma, leading to interventions that do not respect the inherent neurodiversity of the individual. Instead of providing support that acknowledges and embraces these differences, there's a risk of exacerbating feelings of being misunderstood or focusing on inappropriate goals. Understanding the distinction between neurodivergence and trauma is essential to offering effective care that meets the needs of each individual.
To better serve our clients, we must learn to differentiate these overlapping symptoms and explore how these intersections provide more effective solutions. Trauma and neurodivergence cannot be treated in silos—integrated and individualized care is the key to facilitating effective change.
A study of 687 autistic adults revealed that 72% had encountered sexual assault, other unwanted sexual experiences, or physical assault. Furthermore, 45% of the participants met the criteria for PTSD. Research shows that Autistics have a higher prevalence of PTSD compared to the general population. One study found that 32% of Autistic adults met the criteria for PTSD, a rate significantly higher than that of non-autistic individuals. https://www.psychologytoday.com/us/blog/the-forgotten-women/202207/the-crossroads-trauma-and-autism
Statistical conclusions: Autistics face an increased likelihood of exposure to adversity and violence, leaving them more vulnerable to trauma. The statistics paint a stark picture, but what truly stands out is the unique way trauma intertwines with Autism.
Symptoms like heightened sensory experiences, social withdrawal, and communication struggles can stem from both trauma and Autism. Differentiating the root cause is no easy task, yet it is vital to helping clients on their healing journeys. Adopting a neuro-cognitive perspective ensures we approach each client with compassion and curiosity about their unique experiences and neurobiological makeup.
For Autistic clients with trauma histories, individualized therapeutic approaches are essential. This may include work focused on increasing self-acceptance and unmasking, ultimately leading to more fulfilling lives. However, what about those without a formal Autism diagnosis who display Autistic traits? Their sensory needs and tendencies still need to be considered. This is especially important as sensory differences—hypo- or hypersensitivity to touch, sound, taste, and other stimuli—often dictate which coping strategies will (or won’t) be effective.
Sensory regulation is at the heart of effective trauma intervention for neurodivergent clients. The way clients experience their bodies and the world around them impacts their ability to engage in therapy. Here are key sensory domains therapists should consider:
Touch
Sight
Taste/Texture
Sound (e.g., sensitivity to specific noises like misophonia)
Vestibular (balance and spatial awareness)
Interoception (awareness of internal cues, such as hunger or thirst)
Proprioception (awareness of body position and movement)
Alexithymia (difficulty recognizing and describing emotions)
Identifying how sensory processing differences influence emotional regulation or distress is foundational in developing effective coping strategies. For example, one client may find grounding exercises soothing when they engage their sense of touch. For others, the same techniques may exacerbate their discomfort.
It's crucial to recognize that these differences can also manifest in the vestibular system due to trauma. Additionally, some individuals may experience both trauma-induced vestibular changes and be born with a Sensory Processing Disorder. Therefore, incorporating these differences into treatment is vital for effective coping.
A 2022 systematic review of 70 studies involving nearly 4 million participants found that children experiencing multiple adverse childhood experiences (ACEs) are more at risk of developing ADHD. The research highlighted that even having just one ACE, particularly in females, increases the likelihood of an ADHD diagnosis. An article in Academic Pediatrics identified a strong link between traumatic childhood experiences and ADHD. Participants with two or more adverse events were prone to more severe ADHD symptoms. The study concluded that “children with ADHD have higher ACE exposure compared with children without ADHD.” Additionally, another study suggested that individuals with ADHD are significantly more likely to develop PTSD after traumatic events. https://adhdonline.com/articles/adhd-and-childhood-trauma-unraveling-the-complex-link/ Spencer-Andrea-2021-Psychiatry-Academy-ADHD-and-PTSD-1.20.21.pdf
Statistical Conclusions: The intricate relationship between trauma and Attention-Deficit/Hyperactivity Disorder (ADHD) often creates diagnostic challenges. Symptoms of trauma—hypervigilance, disorganization, impulsivity—can mirror those of ADHD, making it difficult to accurately identify and address underlying issues. On top of this, individuals with ADHD experience a higher risk of multiple forms of victimization, compounding the effect of trauma.
Therapeutic success in this intersection lies in addressing both conditions concurrently through a targeted, tailored approach. For example, implementing strategies to manage ADHD symptoms like attention differences or impulsivity needs to happen alongside trauma-focused work. Ignoring these complexities can create unnecessary barriers to healing.
When meeting with clients who have ADHD, it’s vital to explore trauma history thoroughly. Therapists must also provide psychoeducation to help clients understand the confluence of ADHD and trauma, offering tools that address both their cognitive patterns and emotional experiences.
Renner et al. (2016) conducted a study revealing that adult Autistics experience higher levels of dissociative symptoms compared to neurotypical individuals. Despite these findings, additional research is necessary to better understand the prevalence and characteristics of dissociation in autism. Another study, which included 59 Autistic adolescents aged 12 to 18, discovered that 12.5% of participants exceeded the threshold for dissociative disorders. This study also highlighted a significant link between dissociative symptoms and experiences of childhood trauma. https://neurolaunch.com/autism-and-dissociation/ https://link.springer.com/article/10.1007/s10803-024-06374-7
Autistic individuals are three times more likely to experience dissociative symptoms compared to their neurotypical peers. Dissociation—a feeling of disconnection from one’s body, emotions, or reality—can become a frequent refuge for those dealing with overstimulation or chronic trauma. While dissociation can serve as a survival mechanism, it often poses additional challenges in therapy.
Helping autistic clients recognize dissociation and its connection to their trauma can be life-changing. Stabilization skills rooted in sensory needs are particularly effective for this group. For example, introducing grounding techniques tied to proprioceptive or vestibular input, such as rhythmic movement or deep pressure techniques, can help. But these interventions must align with the client’s specific neurodivergent traits to truly be effective.
This calls for therapist adaptability—our job is not to apply a one-size-fits-all solution but to uncover what stabilization looks like for the individual in front of us.
Another frequent intersection in neurodivergent clients with trauma histories is alexithymia, the inability to recognize or verbalize emotions. Alexithymia disrupts emotional processing and regulation and often goes hand in hand with dissociative experiences. Both conditions involve disruptions in awareness, resulting in a disconnect from emotions and self.
Therapy with individuals experiencing both alexithymia and dissociation demands a recalibration of our neurotypical expectations. Traditional approaches emphasizing verbal expression may fall flat for this group. Instead:
Focus on body awareness activities that foster a connection between physical sensations and emotional understanding.
Use visual or conceptual emotional mapping tools.
Avoid pressuring clients to verbalize emotions in early sessions—acknowledge and honor non-verbal expressions.
Effective treatment involves helping clients build a bridge between bodily sensations and emotional identification while offering tools that allow them to feel safe in these explorations.
Providing trauma-informed care for neurodivergent individuals goes beyond addressing immediate symptoms-it lays the groundwork for self-understanding and acceptance. Addressing sensory, cognitive, and emotional overlaps requires us to create space for clients to explore their identities authentically.
When clients feel seen and understood in their uniqueness, they can move toward deeper self-acceptance. This acceptance forms the foundation for meaningful coping strategies, interpersonal growth, and ultimately, an improved quality of life.
How do we, as therapists, rise to the responsibility of supporting neurodivergent clients with trauma? It begins by committing to continuous education and self-reflection. Are we approaching our clients with sensitivity to their sensory differences, communication styles, and individual histories? Are we actively challenging neurotypical standards that may create limitations in treatment?
The intersection of trauma and neurodivergence is complex, but it’s in this complexity that we, as therapists, hold the greatest potential to create life altering changes.
Check out our CE on Trauma Informed Therapy!
Trauma is a word that has been gaining more attention and importance in our society and in the therapy treatment world. We (therapists) all know what
Exploring the complexities of mental health, the threads of neurodivergence and dissociation weave together in intricate patterns. For therapists,...
Trauma-informed therapy explains the connection between the nervous system and mental health, offering a paradigm shift in treating mental health...