Treating Developmental Trauma: Why Is It Important?
Trauma is a word that has been gaining more attention and importance in our society and in the therapy treatment world. We (therapists) all know what
9 min read
KD HOLMES, LPC, EMDR CERTIFIED, BTTI TRAINED
:
Nov 14, 2024 3:24:27 PM
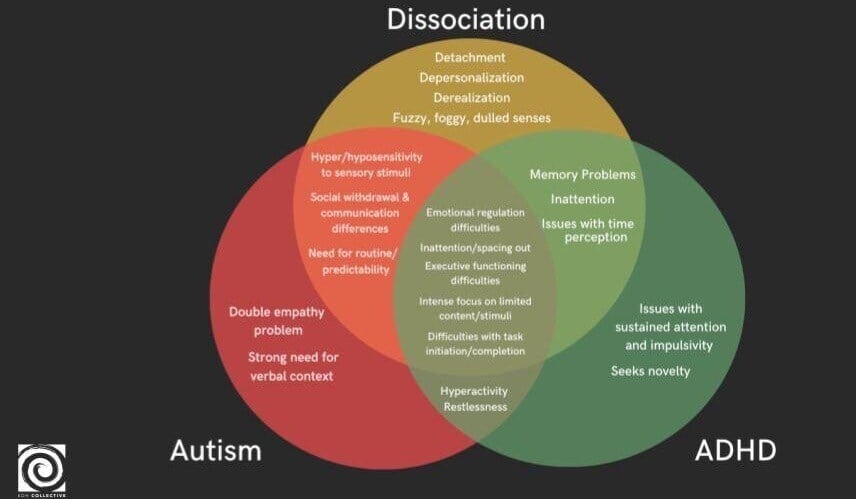
Exploring the complexities of mental health, the threads of neurodivergence and dissociation weave together in intricate patterns. For therapists, differentiating symptoms is difficult and takes time to learn. We are training our minds to observe symptom clusters. This exploration seeks to unravel the nuances of how Neurodivergence, specifically Autism, Sensory Processing Disorder (SPD), and Attention Deficit/Hyperactivity Disorder (ADHD), contribute to dissociation, co-occur with it, or is sometimes mistaken for it.
We've all experienced the moment when we learn about a diagnosis and question whether it applies to us. I recall learning about Borderline Personality Disorder and, in the quiet of my home, calling my best friend with a mix of shame and fear I asked, "Do I have Borderline?" She laughed. Since that time, I have called about Autism and ended up on ADHD. This reaction is quite common; when we learn about something new, we often wonder if we're affected by it and assume all our clients are too.
If you're wondering about the validity of these comparisons, welcome to a place where I once stood. Two years ago, I found myself irritated by it, dismissing it outright. Yet now, it has woven itself into the very fabric of my work, becoming a cornerstone in my approach to mental health. Neurodivergence is a part of the foundation of psychological evaluations, which highlights neurological differences to understand our client's mental health. These evaluations guide my treatment planning, something I call mapping therapy.
Autism, SPD, and ADHD are specific neurotypes within the larger neurodivergent umbrella, each have its own symptom presentation that is common in our office. This high prevalence is especially notable if you are a trauma therapist, which appears to be due to the frequency of these populations experiencing trauma. Research on the experiences of trauma within neurodivergent populations is alarming and should inform how we work.
In the general population, 4.7% are affected by PTSD. Among individuals in high-stress professions, 36% have both PTSD and ADHD (Adler et al., 2004). Regarding Autism and PTSD, 16 to 19% of autistic children and adults are diagnosed with PTSD, while 32 to 60% meet the criteria for PTSD. Let those stats sink in. 😳
When a client exhibits dissociative symptoms which are common in trauma, it's crucial to consider ADHD and Autism diagnosis, as there is a considerable likelihood they have one of these.
The DSM-5 views Autism through a clinical lens, categorizing it as a neurodevelopmental disorder. It highlights challenges like social communication difficulties, restrictive and repetitive behaviors, and sensory sensitivities (SPD). Diagnosis revolves around observable behaviors impacting daily life, with severity levels indicating the support needed. This clinical perspective primarily focuses on deficits associated with Autism.
(Since Sensory Processing Disorder (SPD) is not included in the DSM, the diagnosis is controversial, with sensory differences implying an Autism diagnosis as opposed to being its own diagnosis. While SPD is currently linked with Autism, it can also exist independently, affecting one or multiple senses.)
In contrast to the DSM, a neurodiversity-affirming approach sees Autism as a natural variation in cognitive functioning, embracing both strengths and challenges. This perspective treats these traits as differences in processing, communication, and social interaction-not symptoms needing correction.
Sensory Differences or SPD: Some individuals have a hypo or hypersensitivity to stimuli (sound, touch, light) in their environment or what is known as a Sensory Processing Disorder. These sensory differences also include vestibular and proprioception differences. Autistic individuals experience sensory stimuli in different ways, and the neurodiversity model encourages us to craft environments that honor these differences, rather than viewing them as impairments.
Distinctive Communication Styles: Consider the beauty in direct languages, or a preference for written words. Autistic individuals communicate in diverse ways, and this model urges understanding and respect for these styles, recognizing them as authentic expressions rather than something to correct.
Focused Interests: Picture the joy and mastery that come from diving deep into a beloved topic. The neurodiversity perspective celebrates these passions as strengths, seeing them as sources of expertise and joy, instead of labeling them as "restricted interests."
Nontraditional Social Interactions: Imagine navigating social interactions differently, perhaps with less eye contact or favoring solitude. This model perceives these approaches as natural variations, appreciating the richness they add to human interaction rather than viewing them through the lens of social deficits.
Routine and Predictability: Envision the comfort found in familiar patterns and routines, or perhaps the need for novelty in the day-to-day. The neurodiversity model encourages us to respect these needs and honor self-soothing behaviors, recognizing their role in providing solace and stability.
In the DSM-5, ADHD is depicted as patterns of inattention, hyperactivity, and impulsivity that disrupt daily life or development. It is characterized by challenges in maintaining focus, frequent forgetfulness, restlessness, fidgeting, and impulsive decision-making. The DSM divides ADHD into three subtypes: inattentive, hyperactive, or both.
In contrast, the neurodiversity-affirming model perceives ADHD traits as dynamic elements in the spectrum of human attention, activity, and processing styles, rather than as shortcomings. Picture lively bursts of energy, creativity, spontaneity, and intense engagement with areas of interest. Difficulties with focus or impulsivity are seen not as personal challenges, but as mismatches with typical environments, highlighting the need for support and adaptive strategies that celebrate an individual’s unique strengths instead of enforcing conformity to conventional attention and behavior standards.
Within the DSM-5 framework, it's described as a disruption in consciousness, memory, identity, emotion, perception, or behavior-a response to trauma or extreme stress that ranges from mild "zoning out" moments to severe cases like Dissociative Identity Disorder (DID). Dissociative symptoms, such as depersonalization, derealization, amnesia, dissociative absorption, or fragmented identities, can be poignant reminders of the brain's attempt to shield itself from overwhelming experiences.
Reflecting through the lens of the Neurodiversity-Affirming model, dissociation is less a "disruption" and more a natural, adaptive process-protecting the self in overwhelming situations. This perspective reframes dissociation as an innate survival strategy, recognizing the purpose it serves for those who experience it. This is the genius of the nervous system, highlighting the evolutionary purpose and respecting the role dissociation plays in each person’s experience. It is a part of our resilience and survival.
For neurodivergent individuals' dissociation can be a protective mechanism. In the face of sensory overload or social misunderstandings, dissociation can offer protection from overwhelming experiences.
Symptoms of Autism, SPD, and ADHD can lead to overwhelm and/or heightened vulnerability to overwhelm which can increase dissociative symptoms. While I initially believed this to be the only cause of dissociation, research indicates co-occurrence and misdiagnosis as other possibilities.
Neurodivergence often co-occurs with dissociation, creating a complicated clinical picture. The traumatic experiences of the neurodivergent person can lead to dissociation. Sensory and processing differences can co-occur with dissociation. Recognizing this co-occurrence helps map therapy more efficiently, guiding us with greater precision. It reveals the intricate threads of the clinical picture, allowing us to understand and navigate these complex symptom presentations.
Misdiagnosis is an all-too-common issue when it comes to neurodivergence and dissociation. Autism, ADHD, and SPD might be mistaken for dissociative disorders if clinicians don’t look beyond surface symptoms. Conversely, dissociation might be wrongly attributed to neurodivergence. Let's take a dive into this subject that is often left out of the clinical picture of treatment.
Since there is high co-occurrence of SPD and Autism, consider the difficulties of living daily with heightened senses and sensory processing challenges. What would be the outcome? Sensory overload that triggers a fight-or-flight or shut down response. These challenges often lead to emotional regulation problems and psychological distress, triggering dissociative symptoms. Individuals with SPD and Autism may find themselves having anger outbursts (meltdowns), or mentally "checking out" (shut downs) during sensory overload. Derealization and depersonalization provide a buffer from sensory bombardment.
Research indicates that individuals with SPD and other sensory issues may exhibit heightened dissociative symptoms due to repeated exposure to intense or distressing sensory experiences. This intersection creates a nuanced differences between sensory processing challenges and dissociation, demanding a sensory approach to therapeutic interventions.
The co-occurrence of SPD and Autism and dissociation emphasizes the need for Sensory informed trauma approaches. Addressing both sensory challenges and emotional regulation through sensory integration therapies, reduces the likelihood of dissociation during sensory overload. Because this form of dissociation is triggered by the way an individual experiences and responds to the world. It must be addressed through sensory integration therapies.
Autistic people are more vulnerable to trauma, including but not limited to bullying and social exclusion; as such, co-occurrence is common. Social stressors and trauma intensify emotional dysregulation, potentially leading to dissociation. Understanding these dynamics allows therapists to address every symptom our clients are reporting.
Misdiagnosis can occur when sensory-driven withdrawal or shutdown behaviors in Autism and SPD are mistaken for dissociation. Clinicians unfamiliar with sensory processing challenges may misinterpret these behaviors, leading to incorrect diagnoses. It's crucial to recognize that detachment in SPD stems from sensory dysregulation, not trauma-based dissociation.
Similarly, in Autism, sensory sensitivities and social communication challenges can result in behaviors that appear detached, resembling dissociative symptoms like depersonalization or derealization. However, these behaviors primarily arise from sensory processing issues, not trauma. Understanding these distinctions is essential for accurate diagnosis and effective treatment.
In the realm of trauma and PTSD, disruptions in sensory integration-especially within the vestibular system-can amplify dissociative experiences. This system acts to regulate both external and internal sensory worlds. When it falters, individuals may feel unanchored, drifting from their physical and emotional selves, indicating dissociation. Although this resembles SPD, it is actually a symptom of PTSD. (Just imagine when a client has both😳.)
ADHD and dissociation share overlapping symptoms like attention lapses, memory, "zoning out," time perception difficulties, and emotional dysregulation. However, it's crucial to distinguish between the two. In ADHD, inattentiveness or mental drifting typically stems from challenges with maintaining focus and impulse control. In contrast, dissociation involves a detachment from reality or self, often triggered by trauma or overwhelming stress.
ADHD and dissociation share a bidirectional relationship, each contributing and co-occurring with each other when influenced by trauma and stress. During dissociative episodes, individuals with ADHD might experience intensified symptoms, affecting their attention, memory, emotional regulation, and self-awareness. Additionally, ADHD can contribute to traumatic and stress responses by increases in impulsivity, social challenges, and emotional dysregulation, which heighten distress and often lead to dissociative symptoms. (Envision a cycle where ADHD and dissociation amplify one another.)
Additionally, individuals with ADHD are at a higher risk of experiencing traumatic events, thereby increasing the likelihood of dissociative symptoms. Impulsivity and social challenges associated with ADHD can lead to negative encounters, such as bullying, which contribute to chronic stress and dissociation over time.
Clinicians may misinterpret ADHD-related inattention or emotional detachment as dissociative symptoms, leading to incorrect diagnoses, especially in the absence of a significant trauma history. Both conditions can also show similar responses to sensory stimuli and stress, further complicating diagnosis. Differentiating ADHD from dissociation requires careful examination of the underlying causes of attention issues-whether they stem from neurodevelopmental differences, as seen in ADHD, or from trauma responses, as in dissociative disorders.
Understanding neurodivergence is no small feat! We must delve beyond the surface of what symptoms we observe, where trauma or neurodivergence might be impacting individuals both neurologically and environmentally. Viewing neurodivergence in isolation is like seeing half the picture. Addressing both trauma and neurodivergence is crucial for supporting these vulnerable populations.
Overlapping symptoms of a client’s neurotype and their dissociation can obscure distinctions, leading to misdiagnosis. In clinical settings, there is a tendency to interpret symptoms through a trauma lens, identifying dissociation even in the absence of significant trauma.
Though distinct, symptoms may overlap. An Autistic individual might withdraw from social situations, not due to dissociation, but because of sensory overload. Similarly, the daydreaming associated with ADHD might be mistaken for the fog of dissociation. Recognizing these subtleties is vital to avoid misdiagnosis.
Clients often adopt the language of dissociation through social media's influence. They might not communicate feelings of sensory bombardment or dizziness when closing their eyes, but instead describe sensations of suffocation, being overwhelmed in crowds, shutting down, or avoiding meditation. Even experienced clinicians can observe dissociation without understanding its deeper origins.
Therapists must assess the context of symptoms. Is a client's apparent disconnection from reality due to dissociation or an Autistic shutdown in response to overwhelming stimuli? Contextual understanding aids differentiation, which leads to appropriate solutions, realistic outcomes, and less pathologizing. Acceptance is possible when traits are acknowledged as inherent. In the Neurodiversity-Affirming movement, these traits can also be seen as strengths.
A comprehensive assessment is crucial in preventing misdiagnosis and differentiating symptoms. I love a Psychological Evaluation from a trusted Psychologist. Collaborating with other professionals and gathering family input can improve diagnostic accuracy. I have countless examples of this.
Differentiating between sensory differences in Autism, ADHD, and genuine dissociative symptoms related to trauma, clinicians must conduct comprehensive assessments. By curiously exploring the complexities of each client's experience and neurology, therapists can ensure accurate diagnoses and tailored interventions.
Through trauma-informed and sensory integration approaches, clinicians can address both sensory differences and emotional responses, crafting a comprehensive clinical picture and mapping therapy based on each individual's nervous system. We can create a place where our clients feel heard, understood, and empowered to thrive amidst their sensory differences.
We cannot know everything. The human brain is diverse and shaped by numerous factors. Navigating the complex intersections of neurodivergence and dissociation requires curiosity, intentionality, and a willingness to hold space for clients' nuanced symptomology. By understanding the intricate interplay between Autism, SPD, ADHD, and dissociation, therapists can offer more effective support through tailored interventions. For those wishing to explore these connections further, continuing education and collaboration with peers are invaluable. Let us continue to learn and evolve, ensuring we provide the best care possible for those we serve.
As we continue to explore the intersections of Autism, SPD, ADHD and dissociation, may we hold onto the hope of contributing to the well-being of those navigating these complex tapestries. Together, we can create a network of understanding, acceptance, and solutions that work. The continued enhancements made in our ability to understand the nervous system, and the clinician’s commitment to integrating the latest research into practice, provides an open foundation for our clients to do the same. Let's explore together.
https://www.verywellmind.com/adhd-symptom-spotlight-dissociation-5270278
https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.1015749/full
https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2022.735205/full
https://casereports.bmj.com/content/15/4/e246320
https://childmind.org/article/the-debate-over-sensory-processing/
https://neurolaunch.com/high-functioning-autism-and-dissociation/
https://entivabehavioralhealth.com/autism-and-dissociation-the-connection/
https://psychiatry-psychopharmacology.com/Content/files/sayilar/123/19-24(1).pdf
Sensory Processing Challenges: Effective Clinical Work with Kids & Teens
Trauma is a word that has been gaining more attention and importance in our society and in the therapy treatment world. We (therapists) all know what

For therapists, trauma-informed care is of primary focus in our training and treatment. This approach, characterized by sensitivity to trauma and its...

2025 is here - it's a time for fresh starts, new beginnings, and – let's be honest – a little bit of dreaming. As clinicians, we're constantly...