The Dance of Therapy: Attunement, Undertreating and TIBs
Therapy, at its essence, is like a dance-an ebb and flow of connection, rhythm, and responsiveness. This delicate dance thrives on attunement, the...
11 min read
Jessi LaSalle, MS, LPC : Jul 18, 2024 4:30:59 PM

Exploring the critical role that ethics play in the field of mental health and the impact it has on both professionals and their clients.
For the sake of this blog, we will be referencing the American Counseling Association's (ACA) Code of Ethics.Ethics in mental health is not just a set of rules to adhere to; it is the guiding light that ensures mental health professionals uphold the highest standards of integrity and professionalism. These ethical principles serve as a moral compass, directing professionals to prioritize the well-being and dignity of their clients above all else. By embodying these core values and standards, professionals demonstrate their commitment to excellence and their dedication to providing compassionate and ethical care to those in need. According to American Counseling Association in 2014, "Professional values are an important way of living out an ethical commitment."
Enhancing human development throughout the life span;
Honoring diversity and embracing a multicultural approach in support of the worth, dignity, potential, and uniqueness of people within their social and cultural contexts;
Promoting social justice;
Safeguarding the integrity of the counselor-client relationship; and
Practicing competently and ethically.
In the complex and sensitive field of mental health, ethics play a vital role in establishing trust, fostering a safe therapeutic environment, and promoting positive outcomes for clients. Through ethical conduct, professionals demonstrate their commitment to excellence, respect for autonomy, and dedication to upholding the rights and confidentiality of those they serve.
Ethical practices also protect the rights and dignity of clients, fostering a sense of safety and respect within the therapeutic relationship. They provide a framework for professionals to navigate complex situations and make informed decisions, balancing the needs and rights of their clients with their professional obligations. Additionally, ethical practices help mental health professionals maintain their own integrity and professionalism, ensuring that they act ethically and responsibly in their interactions with clients, colleagues, and the broader community. Ultimately, ethics in mental health is not just a requirement but a moral obligation that guides professionals in their noble mission to help and support individuals facing mental health challenges.
Fostering the right to control the direction of one’s life;
"People subjected to care without their agreement report feeling dehumanized, often with long-term effects on their mental well-being. Coercive practices undermine people’s confidence and trust in mental health services and can stop people from seeking help when they need it," World Health Organization, 2022.
Avoiding actions that cause harm;
"Nonmaleficence is the obligation of a physician (Counselor) not to harm the patient. This simply stated principle supports several moral rules − do not kill, do not cause pain or suffering, do not incapacitate, do not cause offense, and do not deprive others of the goods of life. The practical application of nonmaleficence is for the physician to weigh the benefits against the burdens of all interventions and treatments, to eschew those that are inappropriately burdensome, and to choose the best course of action for the patient," Varkey, 2021.
Working for the good of the individual and society by promoting mental health and well-being;
"The principle of beneficence is the obligation of the physician (counselor) to act for the benefit of the patient and supports a number of moral rules to protect and defend the rights of others, prevent harm, remove conditions that will cause harm, help persons with disabilities, and rescue persons in danger ... The principle calls for not just avoiding harm, but also to benefit patients and to promote their welfare," Varkey, 2021.
Treating individuals equitably and fostering fairness and equality;
"Justice is generally interpreted as fair, equitable, and appropriate treatment of persons...Fairness to the patient assumes a role of primary importance when there are conflicts of interest. A flagrant example of violation of this principle would be when a particular option of treatment is chosen over others, or an expensive drug is chosen over an equally effective but less expensive one because it benefits the physician, financially, or otherwise." Varkey, 2021.
Honoring commitments and keeping promises, including fulfilling one’s responsibilities of trust in professional relationships; and
"Fidelity refers to the faithfulness and loyalty that Counsellors must demonstrate towards their clients. They should adhere to professional commitments, maintaining the trust that clients place in them...Responsibility goes hand in hand with fidelity, as Counsellors must diligently recognize and fulfill their professional duties. It involves being accountable for their actions and taking ownership of their role in the Counselling relationship," Ellis, 2023.
Dealing truthfully with individuals with whom counselors come into professional contact.
"The counselor will always tell the truth regarding their client’s situation and will act accordingly. For example, the counselor communicates transparently with their client if their problem requires more complex treatment, even if this may put them in an uncomfortable position," Aratus, 2022.
The Counseling Relationship
Confidentiality and Privacy
Professional Responsibility
Relationships with Other Professionals
Evaluation, Assessment, and Interpretation
Supervision, Training, and Teaching
Research and Publication
Distance Counseling, Technology, and Social Media
Resolving Ethical Issues
When it comes to upholding ethical guidelines in mental health practice, there are several key considerations that professionals should keep in mind:
Mental health professionals should ensure that clients clearly understand the nature and purpose of the therapy, as well as the potential risks and benefits involved. This informed consent process is crucial in establishing a foundation of trust and transparency in the therapeutic relationship. By providing clients with comprehensive information about the therapy process, including the goals, techniques, and expected outcomes, professionals empower clients to make informed decisions about their mental health care. Additionally, discussing potential risks and benefits allows clients to weigh their options and actively participate in their treatment journey, ultimately leading to a more collaborative and effective therapeutic experience.
Professionals must prioritize the confidentiality of their clients above all else, ensuring that sensitive information shared during therapy sessions remains secure and protected. This commitment to confidentiality not only fosters trust and transparency in the therapeutic relationship but also upholds the fundamental right to privacy for individuals seeking mental health support. Only in rare circumstances where there is a clear legal or ethical obligation, such as when there is a risk of harm to the client or others, should professionals consider disclosing information without the client's explicit consent. By maintaining strict confidentiality protocols, mental health professionals demonstrate their dedication to ethical practice and prioritize the well-being and trust of those they serve.
Maintaining appropriate boundaries is crucial for mental health professionals to uphold the integrity of the therapeutic relationship. By establishing clear boundaries, professionals create a safe and ethical space for clients to explore their thoughts, feelings, and experiences without fear of judgment or exploitation. Dual relationships, where a professional takes on multiple roles with a client, can blur these boundaries and lead to conflicts of interest. Such situations can compromise the objectivity of the therapist and potentially harm the therapeutic process. Professionals need to maintain a level of distance and professionalism to ensure that the focus remains on the client's well-being and growth. By avoiding dual relationships and conflicts of interest, mental health professionals can uphold the ethical standards of their practice and prioritize the best interests of their clients.
Remaining informed about current research, best practices, and ethical guidelines is paramount for mental health professionals to deliver competent and ethical care to their clients. By staying up to date with the latest developments in the field, professionals can enhance their knowledge and skills, ultimately improving the quality of care they provide. Additionally, keeping up-to-date with ethical standards ensures that professionals uphold the highest level of integrity and professionalism in their practice. This commitment to ongoing education and awareness not only benefits clients by ensuring they receive evidence-based and ethical treatment but also reflects the dedication of mental health professionals to continuously improving their practice for the betterment of those they serve.
An example by Whitney Storey, LPC, PMH-C, "I have been deep into the literature on working with autistic folks, and what the literature (and my own experience as an autist) has shown is that cognitive behavioral therapy is ineffective for autists. It is unethical to use traditional CBT with these clients. Acceptance and commitment therapy (ACT) and other mindfulness-based work is showing some promise with autists and has been incredible in helping my own clients in working through their distress."
Maintaining ethical standards in mental health practice can be challenging and may involve various risks. Some potential risks and challenges include:
When mental health professionals have multiple roles with a client, such as being a therapist and a friend, it can lead to conflicts of interest, boundary violations, and compromised objectivity. This blurring of professional boundaries can result in a lack of clarity in the therapeutic relationship, potentially undermining the effectiveness of the therapy. When a therapist takes on a dual role, the client may struggle to differentiate between the therapist's personal and professional personas, leading to confusion and potential ethical dilemmas. Moreover, the therapist may find it challenging to maintain objectivity and provide unbiased support when operating in multiple capacities. Mental health professionals need to uphold clear boundaries to ensure the integrity and effectiveness of the therapeutic process, promoting trust and facilitating the client's growth and well-being.
Social or Personal: Adding clients on social media, engaging socially with a client outside of the therapy session, etc.
Sexual or Improper Physical Contact: Engaging in a sexual or romantic relationship with a client or recently terminated client, sexual or romantic advances towards a client, or utilizing sexual or suggestive language towards a client.
Business or Financial: Engaging in a business partnership or ventures, lending or borrowing money, hiring a client for employment, or giving financial/business advice.
Caretaking and Enmeshment: Feeling the need to "fix" or "rescue" your client or their situation rather than allowing them to develop the skills to work on their own problems. This can look like buying items for clients, reinforcing co-dependent behaviors, inability to set professional and therapeutic boundaries, and taking accountability for your client's shortcomings/mistakes, etc.
Improper Gift-giving or Receiving: Accepting gifts from clients or giving gifts to clients that could potentially influence the therapeutic relationship. Risks include favorable treatment, feelings of manipulation, coercion or exploitation, and skewed decision-making by the client or therapist.
Non-therapeutic Self-Disclosure: Although intentional and thoughtful self-disclosure from a therapist can be a helpful tool in assisting a client, there are areas where self-disclosure by a therapist can be detrimental to the therapeutic relationship. Examples include sharing religious, political, or cultural opinions with a client, utilizing judgemental language, and inappropriate disclosures about a therapist's personal life.
There are instances where mental health professionals may face ethical or legal obligations to breach confidentiality. For example, if a client expresses thoughts of self-harm or harm to others, the therapist may be required to disclose this information to prevent harm and ensure the safety of all individuals involved. In such cases, the therapist must carefully balance the ethical duty to maintain confidentiality with the responsibility to protect the well-being of the client and others. This delicate balance requires thoughtful consideration, ethical decision-making, and clear communication with the client about the limits of confidentiality in therapy. By navigating these challenging situations with sensitivity, professionalism, and ethical awareness, mental health professionals can uphold their commitment to both confidentiality and the safety of their clients.
Examples of Confidentiality Breaches:
Professionals may unintentionally bring their own biases and assumptions into therapy, which can negatively impact the therapeutic relationship and the quality of care provided. It is crucial for mental health professionals to engage in ongoing self-reflection and cultural humility to recognize and address their biases. By acknowledging and challenging their preconceived notions, therapists can create a more inclusive and empathetic therapeutic environment that respects the diverse identities and experiences of their clients. This commitment to cultural competence not only enhances the quality of care but also fosters a deeper level of trust and understanding between the therapist and client. By continuously examining and challenging their biases, mental health professionals can ensure that they provide ethical and effective support to all individuals seeking mental health services.
Mental health professionals may encounter complex ethical dilemmas with conflicting ethical principles or obligations. These situations often require a deep level of introspection, consultation with colleagues, and adherence to ethical codes of conduct to navigate them effectively. By engaging in thoughtful reflection and seeking guidance when needed, professionals can approach these dilemmas with integrity and transparency, ultimately making decisions that prioritize the well-being and best interests of the client(s). Embracing ethical decision-making processes not only upholds the standards of practice but also strengthens the therapeutic relationship and fosters trust between the professional and the client. In facing ethical dilemmas head-on, mental health professionals demonstrate their commitment to ethical practice and the ethical principles that underpin the field of mental health.
National and international mental health organizations provide codes of ethics that outline the principles and standards of ethical conduct for professionals to follow. Other important Codes of Ethics to reference include:
Engaging in regular consultation and supervision with experienced colleagues, supervisors, or professionals is a fundamental aspect of ethical practice in the mental health field. By seeking guidance from individuals with diverse perspectives and expertise, mental health professionals can gain valuable insights and strategies for effectively navigating complex ethical dilemmas and concerns that may arise during therapy sessions. These collaborative discussions not only enhance the therapist's decision-making process but also promote a culture of continuous learning and growth within the professional community. Through open dialogue, reflective practice, and mentorship, therapists can strengthen their ethical awareness and competence, ultimately ensuring the highest level of care and support for their clients.
Some organizations have ethics committees that professionals can consult for guidance and support when facing ethical challenges.
Fostering open and transparent communication with clients regarding ethical concerns is paramount in cultivating a strong therapeutic relationship built on trust and collaboration. By engaging in honest dialogue about ethical dilemmas that may arise during therapy sessions, therapists can create a safe space for clients to express their perspectives and concerns. This open communication not only empowers clients to actively participate in the decision-making process but also promotes a sense of mutual respect and understanding between the therapist and client. Through this collaborative approach, both parties can work together to navigate ethical complexities effectively and find solutions that align with the highest standards of ethical practice in mental health therapy.
Mental health professionals can attend workshops, conferences, and seminars that focus on ethical issues in mental health practice to enhance their knowledge and skills. Engaging in ongoing professional development and training can enhance ethical competence and provide professionals with the knowledge and skills to navigate ethical challenges effectively.
By implementing these strategies, mental health professionals can navigate ethical dilemmas with integrity and prioritize the well-being of their clients.
ON BEING A THERAPIST'S THERAPIST- Monet David, MS, LPC
THE POTENTIAL FOR HARM: ETHICAL CONSIDERATIONS- Monet David, MS, LPC
HURT PEOPLE HURT PEOPLE: WHEN GOOD THERAPISTS DO HARM- Whitney Storey, LPC, PMH-C
WHAT DOES ACCEPTANCE AND COMMITMENT THERAPY HAVE FOR ME - Whitney Storey, LPC, PMH-C
THE IMPORTANCE OF DIVERSITY IN THE THERAPY ROOM - KD Holmes, MS, LPC, EMDR Certified
American Counseling Association. (2014). 2014 ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
Aratus, P. (2022, April 11). Ethical issues in counseling. Do Mental. https://domental.com/blog/ethical-issues-in-counseling#:~:text=Veracity:%20The%20counselor%20will%20always,them%20in%20an%20uncomfortable%20position.
Bridgers, C. G. (2024, May 23). Ethical issues in counseling. Berxi. https://www.berxi.com/resources/articles/ethical-issues-counseling/
Forester-Miller, H., & Davis, T. E. (2016). Practitioner’s guide to ethical decision making (Rev. ed.). Retrieved from http://www.counseling.org/docs/default-source/ethics/practioner’s-guide-toethical-decision-making.pdf
Nora Ellis. (2023, July 28). Ethical framework in counselling: A complete guide. The Knowledge Academy. https://www.theknowledgeacademy.com/blog/ethical-frameworkcounselling/#:~:text=Fidelity%20and%20responsibility,that%20clients%20place%20in%20them.
Snowden, L.R. Bias in mental health assessment and intervention: theory and evidence. Am J Public Health. 2003 Feb;93(2):239-43. doi: 10.2105/ajph.93.2.239. PMID: 12554576; PMCID: PMC1447723.
Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30(1):17-28. doi: 10.1159/000509119. Epub 2020. Jun 4. PMID: 32498071; PMCID: PMC7923912.
World Health Organization. (2022, June 16). Autonomy in health decision-making - a key to recovery in mental health care. World Health Organization. https://www.who.int/news-room/feature-stories/detail/autonomy-was-the-key-to-my-recovery
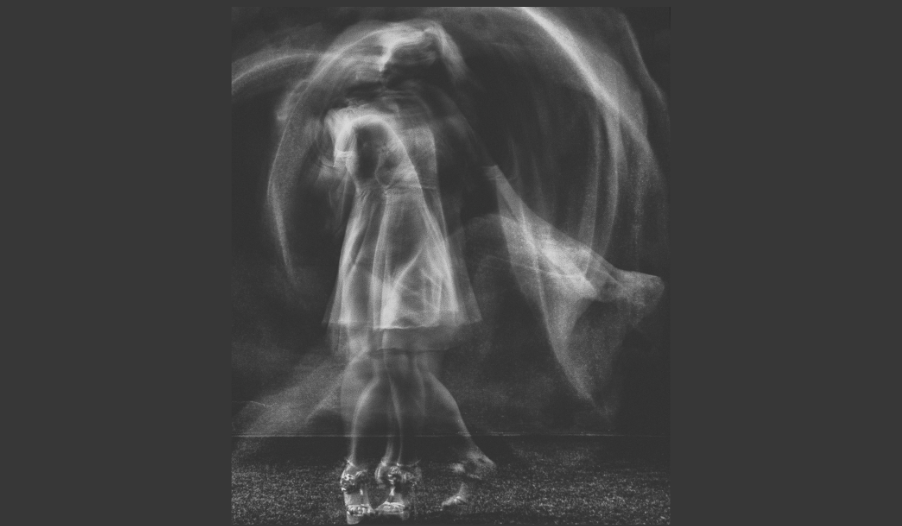
Therapy, at its essence, is like a dance-an ebb and flow of connection, rhythm, and responsiveness. This delicate dance thrives on attunement, the...

Cults have a strange allure. Like many others, I find myself riveted by shows and documentaries that explore their dynamics. There is disbelief,...

In the hushed confines of therapy rooms, where whispered truths echo and one's inner world unfolds, therapists often find themselves facing an...