Riding the Waves of ERP: When Therapy is the Storm
There’s a particular kind of quiet that settles over the room when a client understands ERP and agrees to an exposure for the first time. It’s not...
5 min read
KD HOLMES, LPC, EMDR CERTIFIED, BTTI TRAINED
:
Jan 26, 2025 2:37:06 PM
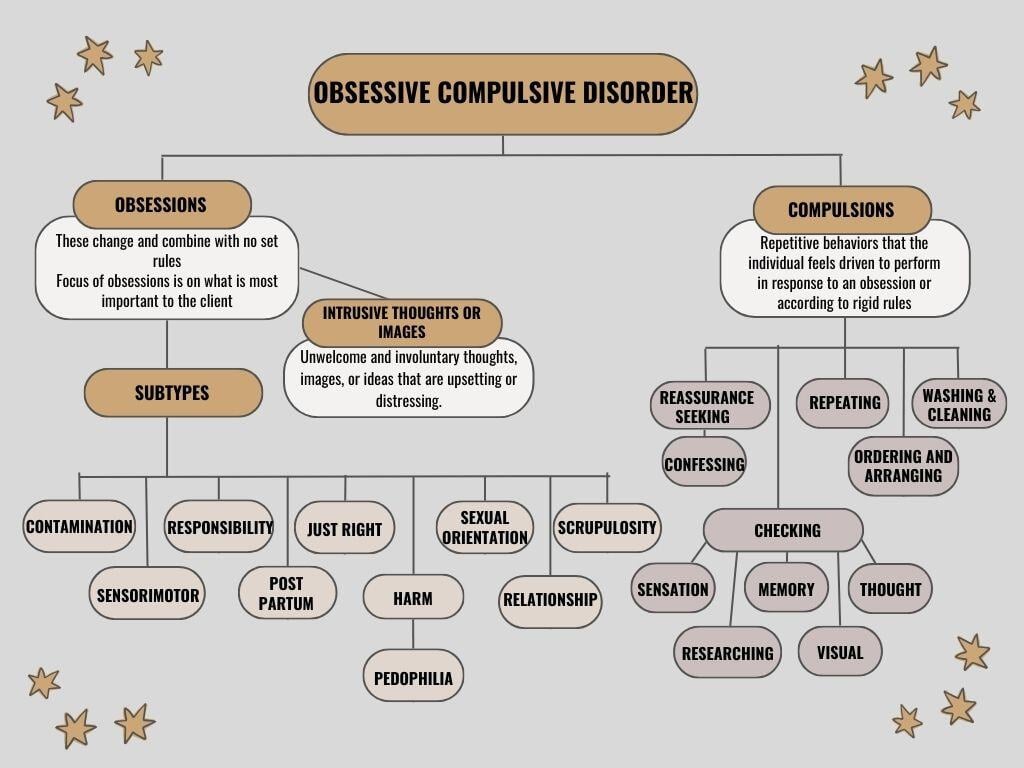
Obsessive-compulsive disorder (OCD) presents itself in nuanced, multifaceted ways. Subtypes of OCD can be conceptualized based on the nature of a client’s obsessions and compulsions (repetitive behaviors). Although every individual’s experience is shaped by their context, emotions, values, and stressors, exploring these subtypes can offer a deeper awareness of the patterns that sustain OCD’s grip on their lives.
Understanding these categories helps therapists design exposures for treatment. When I say exposures, I am referring to Exposure and Response Prevention (ERP) therapy, which is the gold standard treatment for obsessive-compulsive disorder (OCD). ERP works by gradually exposing individuals to their fears or triggers while abstaining from the compulsive behaviors. This method creates new learning to inhibit the old OCD learning ultimately creating freedom from OCD. Understanding these categories, is the first step in treating OCD.
This subtype reflects a search for purity or safety-a need to physically or psychologically disconnect from perceived danger.
Therapist Tip: Shift the lens of focus from external germs to the internal distress they represent. Use Exposure and Response Prevention (ERP) to help clients tolerate the discomfort of not performing compulsions.
Imagine living with the debilitating fear that one minor oversight could lead to catastrophe. For those with Checking OCD, this fear governs their daily life.
Therapist Tip: Reframe the relationship with uncertainty. Help clients recognize that it’s their intolerance of doubt-that perpetuates their checking cycles. Teaching our clients to tolerate the uncertainty of "danger" .
For these clients, feeling just right is necessary for inner peace.
Therapist Tip: Attune to the deeper emotional drivers. Explore how disordered external chaos may mirror clients’ discomfort with disorder within and use ERP to break perfectionistic cycles.
Silent suffering wrestles internally with taboo or distressing thoughts.
Therapist Tip: Normalize thought content without assigning danger to its presence. Use ACT (Acceptance and Commitment Therapy) alongside ERP to teach clients to accept, rather than fight, the fleeting nature of unwanted thoughts.
For clients with Harm OCD, even benign objects or situations are transformed into overwhelming threats.
Therapist Tip: Unpack avoidance behaviors. Gradually expose clients to tools, and build an acceptance of intrusive thoughts without yielding to safety behaviors (compulsive behaviors).
ROCD takes the vulnerability of love and attachment and twists it into relentless questioning and doubts.
Therapist Tip: Guide clients away from resolution-seeking, reinforcing the idea that certainty in relationships is neither attainable nor necessary for healthy love.
For individuals with Sexual OCD, intrusive sexual thoughts do not reflect attraction or desire but evoke deep discomfort and fear.
Therapist Tip: Defuse the stigma around intrusive thoughts. Foster an environment free of shame where clients can openly discuss fears and engage in ERP to confront, rather than evade, their triggers.
This involves intrusive, unwanted thoughts or fears about inappropriate sexual behavior, which can cause significant distress.
Therapist’s tip: Gradually exposing your client to their triggers while teaching them to refrain from compulsive behaviors, helping to reduce their power over time.
Clients with this subtype take moral integrity or religious adherence to extreme, debilitating levels.
Therapist Tip: Collaborate with spiritual leaders if appropriate, and help clients explore the difference between spiritual devotion and compulsive behaviors that stem from fear rather than faith.
For some, the vastness of existential questions becomes a mental trap rather than a source of wonder.
Therapist Tip: Redirect clients to the present moment through mindfulness techniques while teaching them that some questions are meant to coexist with curiosity, not certainty.
This subtype traps clients in an endless loop of focusing on involuntary bodily processes.
Therapist Tip: Interrupt hyperawareness cycles with refocus exercises that ground clients in external stimuli rather than internal sensations.
A subtype of OCD where individuals become obsessed with the fear that they have caused or been involved in an event that never actually happened.
Therapist TIP: Focus on exposing clients to the uncertainty and discomfort of the intrusive thought without seeking reassurance or engaging in compulsions. This helps train your brain to tolerate uncertainty and reduces the power of the obsession over time.
involves obsessive thoughts and guilt over past actions or events. Individuals may fixate on whether they acted appropriately or morally in certain situations, often replaying the event in their minds and doubting themselves repeatedly.
Therapist TIP: Focus on gradually exposing yourself to the thoughts or memories causing distress without engaging in compulsive behaviors. This helps you build tolerance to the anxiety and reduces the need to seek reassurance.
This form of OCD involves persistent doubts or intrusive thoughts about past actions, decisions, or events, often leading to excessive rumination and a need for reassurance.
Therapist TIP: Focus on gradual exposure to intrusive thoughts while resisting the urge to ruminate or seek reassurance. This approach helps reduce anxiety over time and builds resilience.
A condition that can affect new parents, causing intrusive thoughts and compulsive behaviors related to the safety and well-being of their baby.
Therapist Tip: Gradually expose clients to triggering thoughts or situations while resisting the urge to perform compulsions.
OCD may wear different masks, but at its core, it capitalizes on clients values and core fears. For therapists, understanding these subtypes empowers you to empathize, strategize, and intervene with greater precision.
Remember, individuals with OCD often battle shame, confusion, and isolation due to the nature of their thoughts and behaviors. Your role is not only to teach them skills for managing symptoms but also to help them reclaim their lives from a condition that distorts their perception of reality.
Normalize, Normalize, Normalize-let's break the stigma around OCD, the 4th most common mental health condition affecting millions of people worldwide. It's important to understand how OCD works and to avoid unintentionally becoming part of their OCD loop. Sometimes, what we think is helping can actually reinforce their OCD. By educating ourselves, we can provide support and guide them towards real change through ERP.

There’s a particular kind of quiet that settles over the room when a client understands ERP and agrees to an exposure for the first time. It’s not...

Obsessive-Compulsive Disorder (OCD) is characterized by persistent, unwanted obsessions and repetitive compulsions. According to the Diagnostic and...
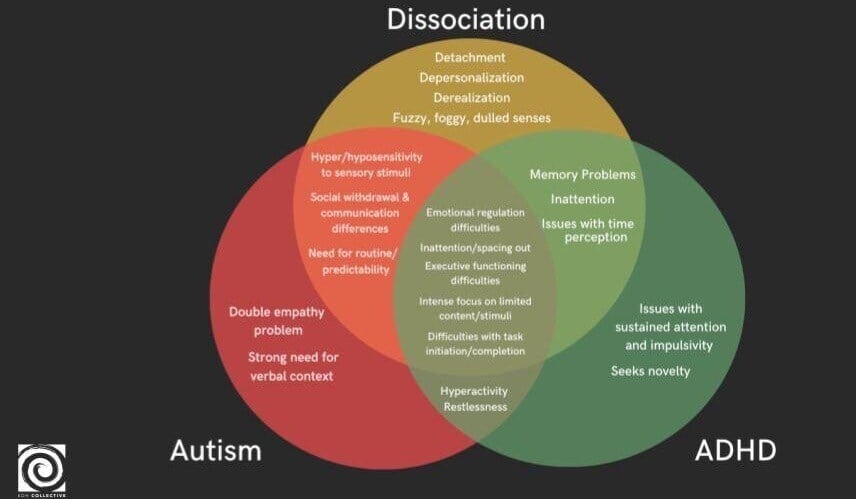
Exploring the complexities of mental health, the threads of neurodivergence and dissociation weave together in intricate patterns. For therapists,...