Who am I, and how the hell did I get here?
“Who am I, and how the hell did I get here?” Life has a way of pushing us toward answers we didn't know we needed. For me, the search for "who I am"...
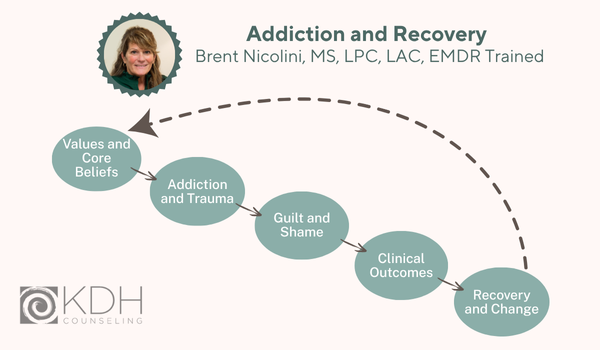
Addiction is one of those words that carries a heavy weight, often misunderstood and loaded with judgment. I've been asked countless times, "What is addiction?" It's never a simple answer, because addiction itself is anything but simple. It's a complex beast with many faces, touching every part of a person's life—their mind, body, and spirit. So let's dive deep into addiction, exploring how different medical and recovery communities define it, diving deep into its impact on our deepest values and sense of self, and uncovering the very real clinical challenges it presents. More importantly, we'll walk through the basics of addiction in order to understand the profound truth of recovery, proving that a life beyond addiction isn't just a dream, but a powerful, achievable reality.
One of the most significant shifts in understanding addiction came from the medical community, moving it from a moral failing to a legitimate illness. The first significant step in this direction within the American medical establishment was in 1956, when the American Medical Association (AMA) officially declared alcoholism an illness. This was a monumental moment, challenging centuries of societal views that often condemned those struggling with alcohol as weak-willed or morally corrupt. By classifying it as an illness, the AMA paved the way for alcoholism to be treated within general hospitals, recognizing it as a condition requiring medical care rather than just punishment.
This foundational concept was further solidified and expanded over the decades. In 1987, the AMA, alongside a growing chorus of other medical organizations, officially termed addiction a disease. This expanded recognition acknowledged that the principles applied to alcoholism—its chronic nature, its impact on bodily and mental health, and its need for medical intervention—were applicable to a broader range of substance dependencies. This broader consensus truly cemented the "disease model" in mainstream medicine.
Then, in 2011, the American Society of Addiction Medicine (ASAM) joined forces with the AMA, not only affirming addiction as a disease but specifically defining it as a chronic brain disorder. This wasn't just a semantic update; it reflected significant advancements in neuroscience. Research had increasingly illuminated how addiction fundamentally alters brain circuits responsible for reward, motivation, memory, and self-control. This shift in terminology underscored the biological underpinnings of addiction, emphasizing that it's not simply a matter of choice or willpower, but a condition rooted in physiological changes within the brain. The implications of this are profound: if it's a brain disease, then it should be treated with the same seriousness and long-term care as other chronic diseases like diabetes or heart disease, and those afflicted deserve access to evidence-based medical treatment.
The official ASAM definition articulates this complex reality: “Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences” (www.ASAM.org). Let's break down this powerful statement. "Treatable" offers immense hope, signaling that recovery is not only possible but medically supported. "Chronic" acknowledges its persistent nature, much like diabetes or asthma, meaning it can be managed but often requires ongoing attention. The phrase "complex interactions among brain circuits, genetics, the environment, and an individual's life experiences" highlights the multifaceted etiology of addiction, moving beyond simplistic explanations. It acknowledges that a person's biological predisposition, their upbringing, their social circumstances, and traumatic events can all play a role in its development. Finally, the core behavioral manifestation – "compulsive and often continue despite harmful consequences" – captures the defining characteristic of addiction: a relentless drive that overrides logic, reason, and self-preservation.
While the medical community focuses on the physiological and neurological aspects, other definitions offer equally critical insights into the lived experience of addiction. Organizations like Alcoholics Anonymous (AA), with its vast global fellowship, define addiction as a three-fold illness: a physical sensitivity to a substance, a mental obsession with the substance, and a spiritual malady. This perspective, born from the shared experiences of recovering individuals, speaks to the holistic devastation of addiction.
The "physical sensitivity" aspect refers to how an individual's body reacts uniquely to the substance, often developing tolerance and experiencing severe withdrawal symptoms, setting them apart from social users. It’s not just a bad habit; their body chemistry responds differently, leading to a compulsive need for more.
The "mental obsession" describes the relentless, intrusive thought patterns that dominate an addict's mind. It's that "hamster wheel" I know so well—the constant strategizing, planning, and rationalizing centered around getting and using the substance. Even when the substance isn't present, the mind is consumed by it, making clear thought and rational decision-making nearly impossible.
And perhaps the most profound aspect for many in recovery, the "spiritual malady," speaks to a deep sense of emptiness, isolation, and disconnection from oneself, others, and any sense of purpose or meaning beyond the substance. It's the erosion of core values, the loss of integrity, and the pervasive feeling of being separated from the "good person" they once were or aspired to be. This spiritual void often drives the continued compulsive use, seeking to fill an unfillable emptiness with the temporary oblivion of the substance.
AA views addiction as a progressive, incurable disease that can be arrested, but not cured. "Progressive" means it inevitably worsens if left untreated. "Incurable" does not mean hopeless; rather, it implies that once a person crosses the line into addiction, they cannot safely return to controlled use. The idea is that the predisposition remains. However, it can be "arrested," meaning the symptoms can be put into remission through sustained abstinence and a program of recovery, leading to a life of sobriety and fulfillment.
Finally, there are the definitions that come from the diagnostic criteria used by mental health professionals. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR – the latest version) moves away from the older terms like "abuse" and "dependence" to a more encompassing concept: Substance Use Disorders (SUDs). The DSM-5-TR states that SUDs (addictions of varying substances) are characterized by patterns of symptoms resulting from persistent use despite negative consequences. This clinical framework allows for a standardized diagnosis and helps professionals assess the severity of a person's struggle, which can vary from mild, moderate, to severe.
The DSM-5-TR outlines 11 specific criteria for SUDs, which fall under four broad categories: impaired control, social impairment, risky use, and pharmacological criteria. These criteria provide concrete, observable behaviors and experiences that indicate the presence and severity of a substance use disorder. Examples of these criteria include:
Taking the substance in larger amounts or for longer than intended: This signifies a loss of control, where a person's usage escalates beyond their initial intentions, a common hallmark of addiction.
Trying to cut down or stop use but failing: Repeated, unsuccessful attempts to control or cease substance use illustrate the compulsive nature and the deep grip the substance has.
Spending a lot of time getting, using, or recovering from substance use: Addiction consumes a person's life, diverting time and energy away from productive activities and towards the pursuit of the substance.
Craving or strong urges to use the substance: These are intense, often overwhelming desires that can make resisting use incredibly difficult, even painful.
Neglecting responsibilities at work, home, or school due to substance use: The substance takes precedence over essential life obligations, leading to functional impairment.
Continuing to use despite causing problems in relationships: Despite the clear negative impact on loved ones, the compulsion to use persists, reflecting the distorted priorities of addiction.
Giving up social or recreational activities because of substance use: Hobbies, social gatherings, and other fulfilling activities are abandoned in favor of substance use.
Using substances in dangerous situations: Engaging in hazardous behaviors while intoxicated, such as driving or operating machinery, demonstrating a profound disregard for safety.
Continuing to use despite knowing of physical or psychological problems caused or worsened by the substance: Even with awareness of severe health consequences, the compulsion to use remains stronger than the desire for well-being.
Developing tolerance (needing more of the substance for the same effect): The body adapts, requiring increasing amounts of the substance to achieve the desired effect, fueling escalation of use.
Experiencing withdrawal symptoms when not using the substance: The body becomes physically dependent, reacting with uncomfortable or painful symptoms when the substance is absent, compelling continued use to avoid these effects.
These various criteria provide a clinical roadmap for understanding the progression and manifestation of SUDs, offering a standardized approach to diagnosis and treatment planning.
My definition combines all of these definitions along with my own experiences with addiction. I am in recovery myself and have been for fifteen years. If I had to put my definition in one sentence it would be this: addiction is an obsession despite negative consequences and the inability to control or stop use. I realize it’s a short definition, but the key concepts are obsession and inability to stop. I do believe it is a disease as it changes brain functions, which affect everything else - physically, mentally, and spiritually. People will use to their death, despite the consequences, because the brain has been trained to use no matter what. It’s a difficult thing to describe unless you’ve experienced it. Every focus and thought is based on the obsession to use. I didn’t think about the consequences because I could override those thoughts with continued use. It was a hamster wheel of continued thoughts of how to use, when to use, how to get the money to use, how to hide the use, why I needed to use, and so on. It was a perpetual thought process focused only on me and how to get and stay high. Nothing else mattered and if it got in the way, I would just use to dismiss the thought.
It’s funny how, while in the depths of addiction we go against every core values and core beliefs we were taught in childhood. Core beliefs as defined by Dr. Jane Mimms (2020), serve as “the bedrock of our existence, entrenched in the very fibers of our identity. They are the profound convictions we hold about ourselves, others, and the world at large. They shape our perspective, coloring our interpretation of reality”.
Core values on the other hand help us prioritize what truly matters in our lives. They empower us to make decisions that align with our authentic selves, guiding us toward fulfillment and contentment. These beliefs and values were taught by someone important to us. Perhaps someone in our family, a coach at school, or a trusted mentor taught us about these values. My grandmother always taught me “not to steal.” My mother taught me “to be honest” and my father taught me the value of good work ethic. It’s funny how all of those beliefs and values went to the wayside while in my addiction. As a matter of fact, I stole from the very person who told me not to steal! Continued use was my only way to deal with my injustices and loss of moral compass. I was doing things that went against everything I had been taught to be “a good person.” I had disrupted the moral code that I had lived by for most of my childhood. Addiction stole those codes from me and the only way I could feel even slightly human, was to use.
Core beliefs are the foundation of our existence, ingrained in the core of our identity. As stated by Dr. Mimms, they are the profound convictions we hold about ourselves, others, and the world at large (2020). They shape our perspective and our interpretation of reality – it is our ideas of self-worth, trust in others, and understanding of societal norms, influencing every corner of our lives. It is important to note that core beliefs and values are what we navigate our lives around. I always said that life was just a bunch of experiences, and how we navigate through them is how and where we end up.
Often times when we move away from our core beliefs and values, guilt and shame arise. This guilt and shame propel the addict/alcoholic to have low self-worth and esteem along with self-condemnation. The lack of trust ensues, and the addict/alcoholic finds it extremely difficult to accept the consequences of their poor decision making. Remember that poor decisions come from lowered inhibitions and the inability to grasp reality while being high. It is very difficult to make well-informed and rational decisions while on a three day meth bender. While the addict struggles to maintain a life of freedom, they unfortunately are living by the grasps of their addiction, which is the opposite of freedom. It’s like an anchor tied to the ankle which the addict must carry each day through life. It is NOT freedom; it is being owned by your substance of choice. Guilt and shame are the number one reasons the addict continues to use because they make them feel numb to feelings of unworthiness and doubt. Trust me, “addicts” know the stigma attached to that name and it creates a trickle effect of continued use. It’s quite sad because it’s a difficult label to squeeze out of when being ridiculed most of the time. This is why it is so important to get help from people who understand the multifaceted aspects of addiction! Support is the cornerstone of asking for help and addicts sometimes don’t know how to ask for help.
This phase of addiction addresses the wide-ranging health consequences that often arise when substance use goes unaddressed, showing up as various physical and mental health issues. It's an important area to understand because addiction often comes hand-in-hand with, makes worse, or even directly causes other serious health conditions. This close link between substance use and mental health is what professionals often call "co-occurring disorders" or "dual diagnosis," and it highlights how addiction can influence a person's entire well-being.
Many individuals struggling with substance use also have earlier diagnoses of conditions like depression, anxiety, schizophrenia, bipolar disorder, and various personality disorders. The connection between mental health and addiction can show up in two main ways:
Sometimes, people with mental health conditions that haven't been treated or diagnosed turn to substances to cope. Imagine someone dealing with ongoing anxiety: the immediate calming effect of alcohol or certain medications might offer a temporary, though risky, break from their overwhelming worries. Similarly, a person experiencing the deep lows of depression might seek the temporary lift from stimulants, or someone coping with intrusive thoughts or hallucinations from schizophrenia might use substances to try and quiet their mind or escape their reality.
This self-medication, while understandable in its effort to ease discomfort, can become a challenging cycle. The substance provides brief relief but ultimately keeps the person from getting proper, effective treatment for their underlying mental health condition. Instead, it can create a cycle where the substance temporarily eases the pain, but its continued use only makes the mental health symptoms more pronounced over time, leading to a greater reliance on the substance and further progression of the addiction. It's like trying to put out a small fire by adding fuel – it just makes the problem grow.On the other side, ongoing and heavy substance use can directly lead to new mental health concerns or make existing ones considerably worse. The brain is incredibly adaptable, but it's also quite sensitive to foreign chemicals. When substances enter the brain, they can upset its delicate chemical balance, affecting mood regulation, thought processes, and how a person perceives things over time.
Consider how specific substances can influence things:
Alcohol: As a depressant, consistent alcohol use can significantly deepen feelings of sadness and depression. While a drink might seem to numb sadness at first, alcohol actually changes brain chemistry in ways that reduce mood-regulating chemicals like serotonin, leading to more lasting and intense depressive states. The American Society of Addiction Medicine (ASAM) clearly states that a "problematic pattern of alcohol use will lead to clinically significant impairment or distress." This impairment often includes a worsening of mood challenges. In fact, studies consistently show a clear link between Alcohol Use Disorder and Major Depressive Disorder, making it essential to treat both conditions together.
Stimulants (e.g., Methamphetamine, Cocaine): These substances can bring on or greatly increase anxiety, paranoia, and even episodes of psychosis. For instance, people struggling with schizophrenia might initially choose stimulants because the intense focus they provide can, for a moment, seem to help with auditory or visual hallucinations. However, with heavy use, these same stimulants can dramatically increase those very hallucinations, leading to heightened paranoia, confused thinking, and a disconnect from reality. The strong anxiety and agitation felt by consistent methamphetamine users can be very difficult to manage, leading to panic and avoiding social situations.
Opioids (e.g., Heroin, Prescription Painkillers): While often used to ease physical pain, ongoing opioid use can lead to notable mood shifts, including feelings of sadness and anhedonia (the inability to experience pleasure). This anhedonia can make recovery feel very challenging, as the brain's natural reward system may be altered, making everyday joys seem dull and unappealing without the drug.
Post-Traumatic Stress Disorder (PTSD): This is a particularly common co-occurring condition. People who have experienced trauma often turn to substances to cope with flashbacks, nightmares, and emotional struggles. However, substances often prevent healthy ways of dealing with trauma, frequently leading to more pronounced PTSD symptoms, increased emotional numbness, and a cycle of avoidance that keeps both conditions active. It's quite common for these two to exist together.The health outcomes connected to addiction highlight a key point: effective treatment for substance use disorder almost always needs to address any co-occurring mental health conditions at the same time. These issues are closely tied, and addressing one without the other can be less effective. For example, using appropriate antidepressants or anti-anxiety medications can help stabilize a person’s mood, easing the strong urges and psychological discomfort that might otherwise lead them back to substance use. Similarly, medications for psychosis can help manage symptoms for individuals with schizophrenia, making it possible for them to engage in therapy and develop coping skills without being overwhelmed.
Overlooking these clinical aspects of addiction would be an incomplete way to understand its influence. It’s not just about stopping the use of a substance; it’s about supporting the entire person – their physical health, their mental well-being, and their core sense of self – to open the door to lasting freedom.
This is the phase where I get very excited to do the work with my clients! To witness an individual facilitate change in their lives and learn to live a life beyond their wildest dreams is one of the most beautiful things in my work as a counselor. This is the phase where people begin to change by asking for help.
Help can look like many different things, but the most important one is just asking for it. Once free from the stronghold of addiction and self-sabotage, we can begin to practice those things that are important to us, like honesty and integrity. We may have to learn or re-learn them, but I promise you will begin to live by those same values and beliefs learned as a child. Everything we need for change is already in us, but through the use of substances we have masked who and what we believe in. When we seek help we begin to adjust our sails to learn how to navigate through life again with the values and core beliefs that we learned a long time ago.
Therapy and self-help groups can help the addict/alcoholic achieve true freedom from the anchors of addiction. I will testify that this is one of the hardest things an addict will do – to facilitate change and recover from the bondages of addiction, but I promise you (that’s two promises so far) that it is the most rewarding experience in life! True freedom is indescribable.
American Society of Addiction Medicine. (2019). Definition of Addiction. Rockville Pike, Suite 200, Rockville, MD 20852
Alcoholics Anonymous. (2014). Alcoholics Anonymous: Big book reference edition for addiction treatment.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-V. Arlington, VA. American Psychiatric Association.
https://www.gildcoaching.com/understanding-core-values-vs-beliefs/

“Who am I, and how the hell did I get here?” Life has a way of pushing us toward answers we didn't know we needed. For me, the search for "who I am"...

POCD or Pedophilia OCD is a subtype of OCD where the person experiences distressing intrusive and unwanted thoughts or fears that they might become...

What is Mindfulness? Mindfulness is a concept that has gained significant popularity in recent years, often associated with practices like relaxation...